
The objective of this study was to assess 10-year national trends in patients who undergo distal radius fracture ORIF using a large patient database. Understanding temporal trends in patient comorbidities and risk factors and episode-of-care outcomes can offer insights into the value of treatments rendered to patients, inform patient counseling, and identify areas for future improvement. 10, 11 This is of growing importance as institutions transition toward value-based care initiatives that balance quality and outcomes against costs of care. 9 Distal radius fracture treatment and its associated complications continue to be a source of economic burden on the healthcare system. 8 With surgical treatment of distal radius fractures, the 90-day complication rate is estimated at 4% and the 1-year complication rate is estimated at more than 30%.

Patients with a distal radius fracture have a 14% higher rate of mortality at 7 years after injury compared with the general population, which likely reflects underlying patient comorbidities and frailty. 7Īlthough the injury and treatment are common, distal radius fractures are associated with notable patient morbidity and mortality. 1, 2, 3, 4, 5, 6 The increasing rate of distal radius fracture ORIF has been largely propelled by the advent of volar locking plate technology, which enables angular stable control of articular fragments, allowing for early mobilization. 1 The incidence of distal radius fractures is increasing across all age groups globally as is the utilization of open reduction and internal fixation (ORIF) for the treatment of this fracture. doi:10.1016/j.ijsu.2016.08.Distal radius fractures are the most common upper extremity fractures and occur with a frequency of 16.2 per 10,000 people. The SCARE statement: consensus-based surgical case report guidelines. Treatment of diaphyseal forearm fractures in children. Nonoperative treatment of both-bone forearm shaft fractures in children: predictors of early radiographic failure. The management of forearm fractures in children: a plea for conservatism. A 10-year study of the changes in the pattern and treatment of 6,493 fractures. Surgical exploration is recommended in cases of delayed recovery of nerve function.īoth-bone forearm case report fracture palsy pediatric peripheral nerve.Ĭheng JC, Ng BK, Ying SY, Lam PK. Conclusion: The uncommon occurrence of ulnar nerve palsy after closed forearm fractures in children should alert physicians to maintain a high index of suspicion and to thoroughly evaluate nerve function in children both before and after reduction of forearm fractures. However, in both-bone forearm fractures, management began with observation, with surgical exploration being reserved for non-improving patients. These fractures are commonly managed conservatively by closed reduction, casting, and rehabilitation. We found 14 case reports in the literature with similar case presentations. The patient was admitted and underwent closed reduction with percutaneous elastic stable intramedullary nailing. On follow-up 7 days later, signs of ulnar nerve palsy in the form of decreased sensation in the little finger and weak abduction and adduction of the fingers were present. Examination at our ED revealed intact vascularity and nerve function.

Case presentation: A 10-year-old boy presented to the emergency department (ED) 1 day after sustaining a closed right forearm fracture due to a fall.
#A PATIENT UNDERWENT CLOSED REDUCTION OF A CLOSED FRACTURE HOW TO#
Furthermore, we explored how to best manage such cases and decrease permanent nerve damage through a literature review. Here, we present a case of ulnar nerve palsy complicating a closed both-bone forearm fracture in a pediatric patient. Identification of the type of nerve damage is vital for proper management of this complication.
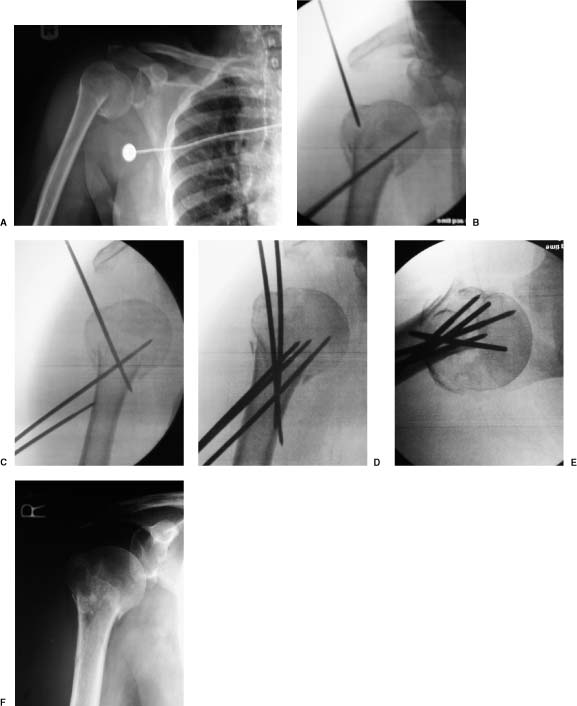
Nerve damage can be due to multiple factors. However, ulnar nerve palsy is a rare complication. Background: Fractures of both the ulna and radius, known as both-bone forearm fractures are common among the pediatric population.


 0 kommentar(er)
0 kommentar(er)
